
An Integrative Health Approach to Chronic Kidney Disease
LETTER FROM WAYNE JONAS, MD

When I was recently asked to speak at a support organization for those with chronic kidney disease, I decided to develop a short one-pager on the topic. However, upon digging into the literature, I quickly realized that the science was so strong that a larger guide was needed to cover the topic properly. This is good news because it means that if you are living with chronic kidney disease, there are a number of effective approaches that you can take to improve your quality of life and prevent your condition from getting worse.
In my more than 40 years as a primary care doctor, I have seen that an integrative approach to most conditions optimizes a person’s ability to heal. This is also true of chronic kidney disease. It is a condition that affects all areas of a person’s life and is highly sensitive to changes in lifestyle. This makes it an ideal condition for whole-person or integrative health care.
When I talk about an integrative health approach, I am referring to a style of care that combines the best of what science and self-care has to offer. This includes evidence-based conventional medical care, complementary medicine, and lifestyle changes to optimize healing.
If you are one of the 37 million people in the United States 1 with chronic kidney disease, read on to explore how an integrative health approach can help. Before you make any changes, talk to your doctor and healthcare team to see what is best for your specific case.
WHAT IS CHRONIC KIDNEY DISEASE?
A diagnosis of chronic kidney disease (CKD) is an indication that your kidneys are damaged and are unable to filter the blood at a normal rate. Kidneys are a vital organ and are responsible for:
- Filtering waste and excess water from the blood, which, in turn, makes urine
- Balancing salt and minerals in the blood to keep your body working properly
- Making hormones to signal the body to make red blood cells
- Keeping bones strong and healthy
It’s normal for kidney function to diminish over time. The amount of kidney tissue you have decreases with age, and the blood vessels that bring blood to the kidneys may harden, which can cause the kidneys to filter waste more slowly. These changes are not necessarily a cause for worry. But the kidneys are not a regenerative organ, and most kidney damage cannot be reversed, so your doctor may want to check your kidney function with blood and urine tests. In its early stages, CKD does not produce any symptoms, and the disease can go undetected until it has advanced. You can also sustain some kidney damage and continue to be healthy since kidneys naturally have a greater capacity than is needed to filter our blood. CKD can eventually lead to end-stage kidney disease (ESKD), which is when the kidneys can no longer function on their own and dialysis or a kidney transplant is necessary. Some patients may choose conservative care over dialysis once they have been diagnosed with ESKD, but this does not prolong life the way dialysis does.
Fast Facts
CKD is more common than you might think, with approximately 15% of U.S. adults, or 37 million people, estimated to have CKD. 2
- It is estimated that 90% of adults who are living with CKD do not know they have it. 3
- CKD is a leading cause of death in the U.S.. 7
- The leading cause of CKD is diabetes: It is estimated that 1 in 3 adults with diabetes will get CKD. 4
- CKD kills more people each year than breast cancer or prostate cancer. 2
- CKD produces no symptoms in early stages and can go undetected until it is very advanced. 2
- CKD patients can reduce their risk of death by 68% if they don’t smoke, are physically active, eat a healthy diet, and have a body mass index of 20 to 25 kg/m. 2 5
More facts on CKD can be found here (PDF).
HOW IS CHRONIC KIDNEY DISEASE DIAGNOSED?
If your doctor suspects you have CKD, or if you are in a high-risk group for developing CKD, your doctor may request the following: 6
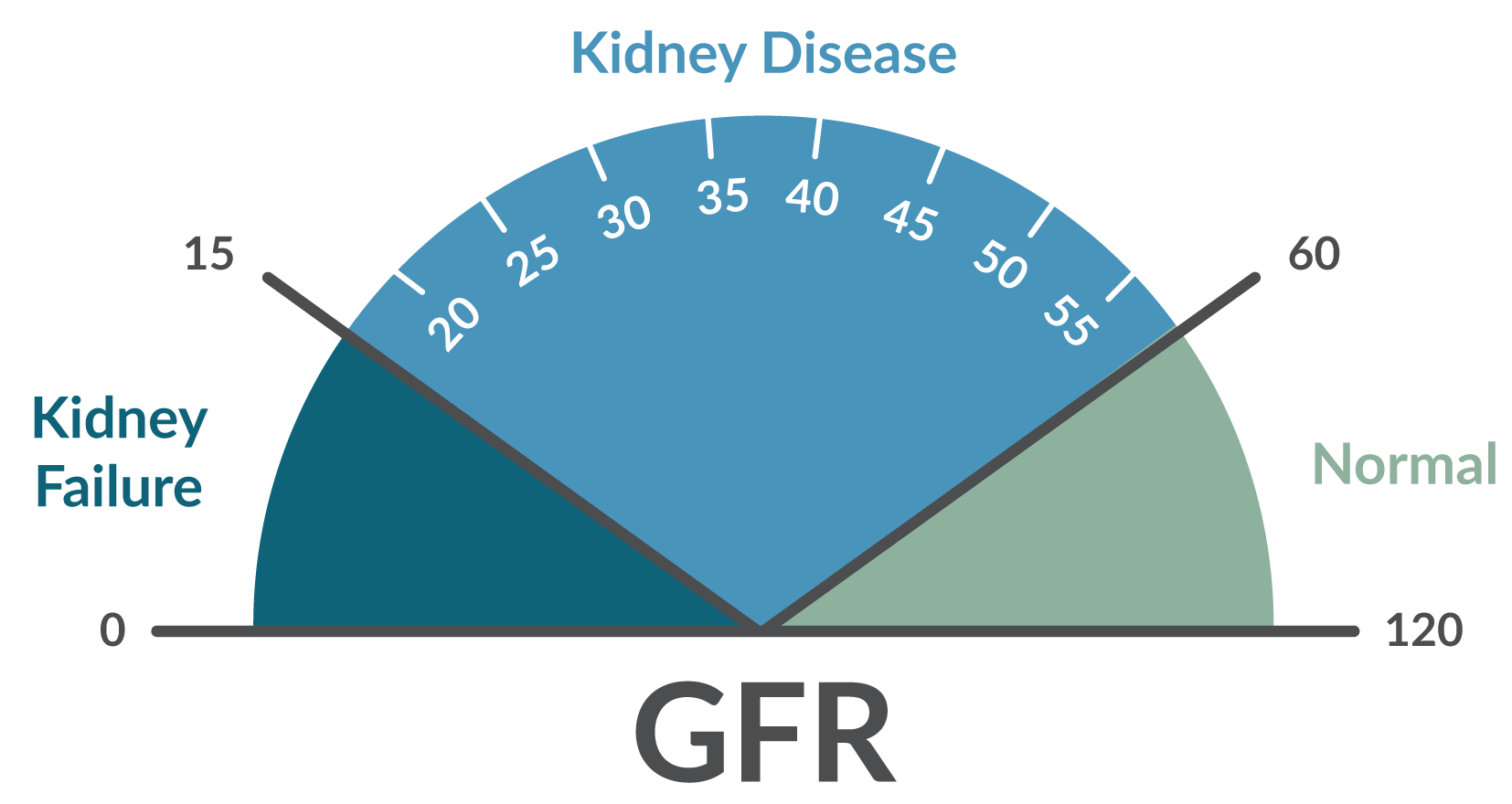
- Blood test — A blood test will measure how much creatinine you have in your blood. Creatinine is a waste product made by muscles that healthy kidneys will filter out effectively. If your kidneys are not working properly, creatinine will build up in your blood. There is a test to help determine your estimated glomerular filtration rate (GFR), allowing your physician to provide more information and insight to the next steps of care.
- The estimated GFR is a measure of how well your kidneys are filtrating your blood of waste products, taking into account your age, sex, body type, and race. If your GFR is below 60 you may have CKD. If you are diagnosed with CKD, the GFR will also help your doctor determine the disease stage.
- Urine test — The urine test will look at the amount of albumin (a protein) and other abnormalities in your urine. Increased levels of protein in the urine for three months or more is an indication of kidney damage. Additionally, analyzing the abnormalities in your urine may also help your doctor understand the cause of your CKD.
It is possible that your doctor may also request imaging, such as an ultrasound, or a kidney biopsy.
WHAT ARE THE STAGES OF CHRONIC KIDNEY DISEASE?
There are five stages of CKD. A great majority of patients will have no symptoms or minimal symptoms until stage 4. Some patients will be able to slow the progression of their kidney damage and will never reach ESKD, and some patients’ kidneys will progress quickly into ESKD. People who are at risk for quick progression and should be closely monitored are:
- Patients with diabetes
- Patients with high blood pressure
- Patients with increasing levels of protein in their urine
- Patients with decreasing estimated GFR
[su_table responsive=”yes” class=”custom-su-table”]
| Stage | Description 7 | GFR (mL/min/ 1.73 m2)* |
|---|---|---|
| 1 | Kidney damage with normal or increased GFR | ≥90 |
| 2 | Kidney damage with mildly decreased GFR | 60-89 |
| 3 | Moderately decreased GFR | 30-59 |
| 4 | Severely decreased GFR | 15-29 |
| 5 | ESKD | < 15 or dialysis |
[/su_table]
*GFR (mL/min/1.73 m2) = glomerular filtration rate in milliliters per minute for 1.73 meters squared
END-STAGE KIDNEY DISEASE
ESKD is the final stage of CKD in which the kidneys can no longer function on their own. It is usually fatal if the patient does not receive dialysis or a kidney transplant within a short period of time. There are a wide variety of symptoms associated with ESKD, including:
- Loss of appetite/weight loss
- Nausea/vomiting
- Overwhelming fatigue
- Insomnia
- Itchy skin
- Shortness of breath
- Metallic taste in mouth/ammonia breath
- Changes in frequency of urination
- Dizziness and trouble concentrating
- Headache
- Skin or nail changes
- Easy bruising
Once diagnosed with ESKD, people need to receive dialysis regularly or a kidney transplant.
WHO ARE THE AT-RISK PATIENTS?
Certain diseases and chronic conditions can put people at risk for developing CKD. If you have been diagnosed with any of the following chronic conditions, your kidney functioning should be monitored.
- Diabetes is the leading cause of CKD. Almost 1 in every 3 people with diabetes has CKD. People with diabetes have high blood glucose levels, which can cause damage to blood vessels in the kidney over time. People should be tested every year if they have type 2 diabetes or have had type 1 diabetes for more than five years.
- High blood pressure (hypertension) is the second leading cause of CKD. Almost 1 in every 5 adults with high blood pressure has CKD. High blood pressure causes damage to the kidney’s blood vessels over time.
- Heart disease and atherosclerosis patients are more likely to develop CKD, and CKD patients are more likely to develop heart disease. If you have been diagnosed with either heart disease or CKD, there is an increased risk of developing the other condition because both have similar causes, such as high blood pressure, diabetes, and high cholesterol levels.
Additionally, people with a family history of CKD are at a greater risk for CKD and should also be tested and monitored. People with genetic diseases (such as polycystic kidney disease and Alport syndrome), autoimmune conditions (such as lupus and vasculitis), obstructions (such as prostate obstruction or kidney stones), and other systemic illnesses (such as myeloma and lymphoma) may also be considered at risk.
Hispanics, Native Americans, and African Americans are at a higher risk of developing diabetes, high blood pressure, and, therefore, CKD. Scientists are studying these groups to better understand if there are additional factors for their increased CKD risk.
LIVING WITH CKD: WHAT ARE THE CONVENTIONAL TREATMENTS?
If you have CKD, there are ways to prevent and slow further kidney damage. Disease progression largely is based on a combination of factors specific to the individual patient. The National Institutes of Health recommends the following strategies for living with CKD. 9
Top 12 Strategies for Living with CKD
- Control your blood pressure
- Control your blood glucose levels
- Monitor your kidney function
- Review your current prescription medications with your physician
- Take medicines as prescribed
- Consult with your physician before taking any over the counter medications or supplements
- Develop a healthy meal plan
- Engage in physical activities
- Maintain a healthy weight
- Sleep seven to eight hours each night
- Don’t smoke
- Develop healthy ways to cope with stress and depression
Control your blood pressure — This is the most important step you can take to prevent further kidney damage. Your blood pressure should be kept below 140/90 mm Hg. Some steps you can take to manage your blood pressure include:
- Instituting a heart-healthy and low-sodium diet
- Quitting smoking
- Being active
- Getting enough sleep
- Taking medications as prescribed
If you have diabetes, meet your blood glucose levels — Check your blood glucose levels regularly to make sure they are within a normal range. This will reduce long-term kidney damage caused by poorly managed blood glucose levels that will increase kidney damage over time.
Work closely with your health-care team to monitor kidney function — As kidney disease tends to get worse over time, it is important to track kidney function and disease progression. To slow disease progression, your goals should be to maintain your estimated GFR and either maintain or lower your urine albumin level. Your physician will also monitor your blood pressure and, if you have diabetes, your blood sugar levels will be monitored with a hemoglobin A1C test. It is recommended you bring this document to your appointments to keep track of your test results.
It is also recommended that when you prepare to meet with your health-care provider(s) that you keep track of questions to ask about your disease and how your lifestyle choices could be having an impact on your CKD progression.
Who makes up your health-care team is up to you, but it may include a number of different healthcare providers to support you in living with CKD, including your primary healthcare provider, a registered dietitian, a nurse, a diabetes educator, a social worker, a psychologist, and/or a nephrologist.
[su_table responsive=”yes” class=”custom-su-table”]
| Sample Questions to Ask Your Doctor |
|---|
| What causes kidney disease? |
| How well are my kidneys functioning now? |
| What treatments do you recommend for my current symptoms? |
| What are the symptoms of worsening disease? |
| How can I reduce my chances of progressing to ESKD? |
[/su_table]
Review your current prescription medications with your physician — Certain medications may cause dangerous drug interactions for CKD patients. Some drugs can prevent your CKD medications from working as they should; others may create severe side effects when combined with your CKD treatments. For example, some antibiotics, antifungal drugs, and diabetes medications may require a change in dosage to prevent kidney damage. You and your physician should review what medications you take to ensure that you avoid any serious adverse interactions.
Take medicines as prescribed — It is very important that you take your medications as prescribed by your health-care providers. Although there is no medication specifically for CKD, taking your other medications appropriately can significantly slow the progression of CKD and kidney failure. Medications your doctors may prescribe include:
- Blood pressure medications: You may be prescribed blood pressure medications even if you do not have high blood pressure because they can slow CKD progression by changing the rate of blood flow to the kidneys. The most common forms of blood pressure medications prescribed for CKD are angiotensin converting enzyme (ACE) inhibitors, such as ramipril, enalapril, and lisinopril, and angiotensin receptor blockers (ARBs). However, these blood pressure medications should be monitored closely by your physician because as the disease progresses and your kidney functioning decreases, blood pressure medication can damage the kidneys.
- Cholesterol medications: You are at a higher risk of heart attack or stroke if you have CKD. Because of this, you may be prescribed statins in a kidney-friendly dosage to reduce your likelihood of developing cardiovascular disease.
- Diuretics: It is possible that your kidneys may have a hard time removing fluids from the blood. This may cause your tissues to retain water, which can cause your ankles, hands, and feet to swell. In addition to reducing your salt intake, you may be prescribed a diuretic to help remove fluids or to lower your blood pressure.
- Medications to address anemia: 10 Your kidneys are responsible for producing and releasing a hormone called erythropoietin (EPO) that signals the bone marrow to make more red blood cells. However, damaged kidneys may not be able to produce enough EPO and, in turn, the bone marrow will not produce enough red blood cells. A lack of healthy red blood cells is called anemia. The two main treatments for anemia caused by reduced EPO production are a subcutaneous injection of a synthetic form of EPO, called erythropoietin-stimulating agent, or supplemental iron pills or injections. Your doctor may also recommend vitamin B12 or folic acid supplements. In rare instances of severe anemia, your doctor may recommend a blood transfusion.
The dose and frequency with which you take medications will change over time as your disease progresses. It is important to follow the instructions given by your health-care provider since your kidneys may have troubling filtering certain medications as your disease progresses, causing an unsafe buildup in your system.
Pay attention to over-the-counter medications — Please consult with your physician and/or pharmacist before taking any over-the-counter (OTC) medications or supplements. Specifically, nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen and naproxen, can damage your kidneys and lead to acute kidney injury. NSAIDs are sold under many different brand names, and you should always check with your physician and/or pharmacist before taking any OTC medications to treat pain.
If you do plan on purchasing and taking OTC medications, here are some tips to avoid complications:
- Keep a running list of all the medications you take (this includes prescription and OTC medications, as well as supplements) in your wallet and bring this list with you to the pharmacy and all your healthcare visits
- Check for any harmful interaction warnings on medication labels
- Always ask your pharmacist how the medication may affect your kidneys or if there may be interactions with the current medications you are taking
- Fill all your prescriptions and purchase all OTC medications at the same pharmacy
Develop a meal plan with a dietitian — Healthful food and drink play an important role in kidney health and can also help you lower your blood pressure, maintain a healthy blood sugar (glucose) level, and delay or even prevent problems caused by CKD. A dietitian can help you develop healthy meal plans and help you meet the goals set by your physician, such as decreasing your sodium intake to reduce or maintain a healthy blood pressure. Additionally, with advanced stages of CKD your dietitian will likely recommend eating foods with less phosphorus and potassium. To learn more about ways you can use food and nutrition to support your CKD, click here.
Introduce physical activity into your routine — Physical activity for 30 minutes a day can help you maintain a healthy weight, reduce stress, and achieve blood glucose and pressure goals. Before you begin regular physical activity, it is recommended you first speak with your health-care provider.
Maintain or strive toward a healthy weight — Being overweight can make your kidneys work harder and may speed up disease progression. Monitoring what you eat (with the help of a dietitian) and exercising regularly can help you reach your weight loss goals and/or maintain a healthy weight to slow CKD progression.
Sleep 7 to 8 hours a night — Getting adequate and restful sleep is important for physical and mental health and can help you maintain a healthy weight and healthy blood pressure and glucose levels.
Don’t smoke — Smoking can increase CKD disease progression and cause damage to the kidneys. Additionally, smoking is associated with increased blood pressure and a greater likelihood of heart disease and stroke, which make it harder to effectively treat CKD.
Cope with your stress and depression in healthy ways — Long-term stress is associated with increased blood pressure, blood glucose, and depression. Mind-body methods such as meditation and mindfulness, maintaining regular physical activity, and getting an adequate amount of sleep can all help with stress reduction. Depression can make it harder to engage in self-care and other activities that can help slow kidney disease progression. Seeking the help of a trained therapist can also help you manage your stress and/or depression.
WHAT ARE LIFESTYLE APPROACHES TO LIVING WITH CKD?
As recommended by the National Institutes of Health, there are many lifestyle approaches that can slow disease progression and make it easier to live with CKD. The three key lifestyle approaches for managing CKD before it progresses to ESKD are diet, exercise, and stress reduction. Remember: Small lifestyle changes can make a big difference in maintaining your kidney function and improving your overall health.
FOOD AND DRINK
Your diet plays a crucial role in CKD disease progression. For all stages of CKD, it is recommended that patients:
- Reduce sodium intake — It is important to choose and prepare foods that are low in sodium, and it is recommended you consume less than 2,300 milligrams of sodium each day. (On average, Americans consume more than 3,400 milligrams of sodium a day.)
- Eat the right amount and the right types of protein — Kidneys remove the waste produced when your body uses protein, so it is important not to eat more than the amount of protein necessary to keep the kidneys from working too hard. This means it is important to eat small amounts of animal- and plant-based proteins. Try to eat a meatless meal for your largest meal (usually dinner) at least once a week.
- Eat heart-healthy foods — It is important to eat foods that are heart healthy to keep fat and calcium from building up in the heart, kidneys, and blood vessels. Learn more about a heart-healthy diet here.
- Limit alcohol consumption — Drinking too much alcohol can cause serious health problems and can damage your kidneys, liver, heart, and brain. It is recommended that men do not drink more than two drinks a day and women no more than one. Consult your health-care providers to understand how much alcohol you can safely consume.
As your disease progresses, it is recommended you also:
- Consume foods with less phosphorus — As your disease progresses your kidneys are less able to filter phosphorus from your blood. When phosphorus builds up in your blood, it pulls calcium from your bones, which causes your bones to become thin and weak and increases their chances of breaking. Your doctor may suggest taking a phosphorus binder, which is a medication you can take with your meals to bind the phosphorus so it does not end up in your bloodstream.
- Consume foods with the right amount of potassium — It is important to consume just enough potassium in your diet to support the proper functioning of your nerves and muscles; too much or too little potassium in your blood can be problematic. When your kidneys are damaged, too much potassium can build up in your blood and cause heart damage. As your disease progresses, you should limit your intake of avocados, oranges, tomatoes, potatoes, and bananas. Also, steer clear of orange juice and tomato juice as they are both high in potassium. Certain salt substitutes and supplements may also contain high levels of potassium, so always check the label and consult with your physician before using. It is also possible that certain prescription medications your physician prescribes may increase your potassium levels. These medications should be tracked over time and adjusted as needed.
To learn more about what to eat and what not to eat when you have CKD, please visit: National Institute of Diabetes and Digestive and Kidney Diseases: Eating Right for Chronic Kidney Disease or National Kidney Foundation: Nutrition in CKD.
Before starting any new diet, seek the advice of a registered dietitian/nutritionist. It is important to continue to see a dietitian since the nutrients and types of foods and drinks you should consume will change as your disease progresses. To learn more about seeking the advice of a registered dietitian, please see this pocket guide on Nutritional Counseling (PDF)
Additional information and tips on how to manage specific nutrients can also be found by clicking here:
Evidence
Adherence to a Western diet, which is characterized by low intake of fruit and vegetables and high intake of animal fat, red meat, ultra-processed foods, and sweets/desserts, is correlated with decreased kidney function and can speed up disease progression in patients with CKD. Studies have also found a Western diet is associated with rapid kidney decline in older adults. 11
A Cochrane Systematic Review including 17 studies (1,639 participants) that looked at the impact of different dietary changes on health outcomes and the well-being/quality of life of people with CKD (including those on dialysis) found that the impact of these dietary changes on mortality, cardiovascular events, and ESKD is uncertain since these measures were rarely reported on in the included studies. However, this review did find evidence that dietary interventions may increase health‐related quality of life and improve GFR, serum albumin, blood pressure, and serum cholesterol levels. 12
MEDITERRANEAN DIET
The Mediterranean diet is a set of guidelines shaped and inspired by the traditional eating patterns of the regions surrounding the Mediterranean Sea and encourages the consumption of lean proteins in small portions, fruits and vegetables, legumes, whole grains, and healthy fats (specifically those high in monounsaturated, polyunsaturated, and omega-3–rich fatty acids).
Evidence
In a prospective longitudinal study called the Northern Manhattan Study (NOMAS), 900 multiethnic participants from northern Manhattan, New York—who were at least 55 years old, had not had a stroke prior to the study, and had no MRI contraindications—were followed from 2001 to 2008. Researchers tracked their kidney and cardiovascular functioning and related outcomes over time and found that dietary patterns similar to the Mediterranean diet were positively associated with kidney function. Specifically, participants with a Mediterranean diet questionnaire score at or above the median had approximately 50% decreased odds of developing incident estimated GFR of less than 60 mL/min/1.73 m2. 13
n another prospective longitudinal study, the dietary patterns and kidney function of 1,212 adults, aged 30 to 71 years, were tracked for six years. The researchers found that there was an inverse relationship between CKD incident risk and adherence to a Mediterranean diet (as assessed by the Mediterranean diet questionnaire score). 14
A randomized controlled trial of 40 ESKD patients with dyslipidemia, hypertriglyceridemia, and/or hypercholesterolemia were randomized to receive either group nutritional counseling based on the Mediterranean diet or usual care. This study found that the nutritional counseling intervention helped improve cardiovascular health by improving the nutritional value of the food consumed, which, in turn, reduced dyslipidemia and protected against lipid peroxidation and inflammation. These improved outcomes allowed the participant to enter dialysis with better cardiovascular health. 15
To learn more about this dietary approach, please click here.
THE DASH DIET
The Dietary Approaches to Stop Hypertension (DASH) diet is designed to prevent and lower high blood pressure. The DASH diet recommends vegetables, fruits, whole grains, fat-free or low-fat dairy products, fish, poultry, beans, nuts, and vegetable oils. The diet limits salt, saturated fat, and sugar.
Evidence
In a prospective before-and-after feeding pilot study of 11 adults with moderate CKD (stage 3), participants completed one week of a reduced sodium diet followed by two weeks of the DASH diet. This study reported the reduced-sodium DASH dietary pattern did not cause acute metabolic events in adults with moderate CKD. Results also indicated that the diet may improve nocturnal blood pressure. The authors concluded that more research was needed to better understand the long-term impact of the DASH diet. 16
The diets and blood pressure readings of 3,135 Black Americans participating in the Jackson Heart Study were monitored over a four-year span (2000–2004). Although the group overall had low DASH scores, better DASH scores among the participants with CKD was associated with lower blood pressure. 17
A longitudinal prospective cohort study following 3,121 women for 21 years found that participants who followed a Western-style diet significantly increased their chances of elevated levels of protein in the urine and a rapid decrease in kidney function.
LOW- OR VERY-LOW-PROTEIN DIET
The most recommended diet for people with CKD is a low-protein diet. Given the stress that digesting protein can cause to the kidneys (which, in turn, can increase disease progression), limiting protein sources can slow disease progression during the early stages of the disease and can prolong time till dialysis.
Evidence
A Cochrane Systematic Review including 17 studies (2,996 participants) that looked at the impact of low-protein diets for nondiabetic adults with CKD (including those on dialysis) found that adhering to a very-low-protein diet likely reduces the number of people with CKD stages 4 or 5 who progress to ESKD. 18 Another systematic review and meta-analysis including nine studies (506 participants) that looked at the impact of a low-protein diet for patients with diabetic kidney disease found that there is a strong relationship between a dietary protein intake of less than 0.8 g/kg of protein and the slowing of GFR decline, as well as decreased levels of protein in the urine. 19
However, low- or very-low-protein diets probably do not influence death in these patients. The data are limited on the effects that low- and very-low-protein diets have on mortality and whether adhering to one of these diets has an impact on quality of life. One review recommends more research on the impacts on quality of life and additional adverse effects of low-protein diets before recommending their widespread
use. 20
EXERCISE
The National Kidney Foundation recommends that people with CKD exercise 30 to 60 minutes a day most days of the week because exercise has been linked to improved outcomes and slower kidney disease progression. Exercise can help you: 21
- Maintain a healthy weight
- Control your blood pressure, glucose, and cholesterol levels
- Prevent heart and disease and diabetes
- Decrease disease-associated stress and anxiety
Proper Exercise
If you are new to exercise and have not previously engaged in regular physical activity, the National Kidney Foundation recommends starting with 10 to 15 minutes a day and gradually working up to 30 to 60 minutes a day. But exercise needs to be done properly, so it’s important to discuss any exercise program with your doctor before you start. Improper exercise can produce:
- Fatigue
- Pain and soreness
- Injuries
- Exercise obsession
- Headaches
Evidence
In a randomized controlled trial, 150 nondiabetic adult patients with hypertension and CKD stages 2 to 4 received either 16 weeks of aerobic and resistance training or usual care. The study found a significant increase in functional capacity on step tests and stand tests and a decrease in high-sensitivity C-reactive protein and fasting blood glucose levels in the exercise group compared with control group. These results suggest that aerobic exercise may reduce inflammation and insulin resistance in patients with early stages of CKD. 22
A systematic review and meta-analysis of 31 randomized controlled trials (including 1,305 participants) on the impact of aerobic exercise on patients with CKD found that adult CKD patients benefit from aerobic exercise training via increased cardiorespiratory function, increased high-density lipoprotein cholesterol level, and improved health-related quality of life. 23
A systematic review and meta-analysis of 13 randomized controlled trials (including 421 participants) on the impact of aerobic exercise on patients with CKD found that exercise therapy may be beneficial for CKD patients not on dialysis by reducing body mass index, systolic blood pressure, and diastolic blood pressure, and by increasing GFR. Additionally, this meta-analysis also found that short-term exercise interventions can decrease triglyceride levels. 24
MANAGING STRESS AND PSYCHOLOGICAL DISTRESS
It is important to find healthy ways to manage and cope with stress to offset the challenges of living with CKD. Long-term stress can also lead to increased blood pressure, which can decrease kidney functioning, increase the likelihood of developing depression, and lead to unhealthy coping strategies that can make it harder to manage CKD. A recent study found that mild to moderate levels of psychological distress were associated with smoking and low physical activity in participants with CKD. Additionally, compared to participants with CKD who reported no unhealthy behaviors, participants with two to three unhealthy behaviors were almost five times more likely to report severe psychological distress. 25
Managing stress and anxiety can become increasingly challenging once a patient has progressed to ESKD and is receiving dialysis regularly; it is estimated that up to 50% of people with ESKD undergoing hemodialysis suffer from anxiety and depression, which results in decreased quality of life. 26 Evidence based ways of effectively coping with and managing stress include mindfulness meditation and behavioral therapeutic interventions, such as music and spiritual therapies and talking to a psychotherapist.
Mindfulness Meditation
Meditation is a practice that involves consciously exerting control over breathing and attending nonjudgmentally to the present moment. It produces multiple physiological and chemical effects, such as decreased heart rate, blood pressure, and cortisol (stress hormone) levels. Meditation is widely considered a safe way of addressing physical and mental symptoms.
Side Effects/Safety Concerns
Although rare, there have been reports that engaging in breathwork has worsened symptoms of patients with psychiatric problems, such as anxiety. If you are attending a breathwork class, please make sure to alert your instructor of any physical or psychological condition you may have.
Excessive, rapid breathing can drop carbon dioxide levels and change the pH of the blood, causing tingling, muscle cramps, light-headedness and, on rare occasions, seizures. If you are susceptible to seizures, consult your doctor before engaging in any type of meditation that includes intensive breathwork.
Evidence
In a pilot, randomized, crossover study, 15 African American men with hypertension and CKD received either a 14-minute educational video on blood pressure (the control) or 14 minutes of mindfulness meditation. Compared with the control video, mindfulness meditation significantly reduced systolic blood pressure, diastolic blood pressure, mean arterial pressure, respiratory rate, and heart rate, and produced a significantly greater reduction in muscle sympathetic nerve activity (MSNA). A subset of participants who received a controlled breathing intervention alone (without the mindfulness meditation) did not experience significant decreases in blood pressure, respiratory rate, heart rate, or MSNA. 27
In a pilot feasibility study, 40 participants with ESKD on hemodialysis were randomized to participate in either a health education program or the same health education program plus eight sessions of mindfulness-based stress reduction (MBSR). Participants who received MBSR had significant reductions in both anxiety and depression over the eight weeks. 28
BEHAVIORAL THERAPEUTIC INTERVENTIONS
Seeking the counsel of a trained psychotherapist and incorporating stress reduction methods are key steps in addressing the challenges associated with CKD. Psychotherapists can help you incorporate coping strategies and new ways to approach living with CKD.
Side Effects/Safety Concerns
Psychotherapy, when delivered by a well-trained certified therapist, is widely considered a safe way of addressing the added stress that managing your CKD can cause. Note that any form of therapy can unearth uncomfortable emotions and may cause you to experience increased levels of psychological discomfort.
Evidence
A Cochrane Systematic Review including 33 studies (2,056 participants) that looked at the impact of psychosocial interventions on preventing and treating depression in people with CKD found that, in addition to exercise and relaxation techniques, cognitive behavioral therapy (CBT) reduced depressive symptoms and increased health-related quality of life. 29
A pilot study of seven participants with ESKD who were undergoing hemodialysis investigated the effects of 12 weeks of group CBT with mindfulness. The authors found that the participants had significant improvements in anxiety, perceived stress, quality of life, and depression after the 12-week intervention. 30
A systematic review including 32 randomized controlled trials looked at the use and application of mind body interventions to address the psychological and physical symptoms faced by people with CKD (including people undergoing hemodialysis). The most studied interventions were music therapy (11 studies), relaxation therapy (nine studies), and spiritual therapy (six studies). Music and spiritual therapies were the most effective for anxiety reduction, and spiritual therapies were the most effective in addressing depression-related symptoms. To relieve pain, music and yoga therapies were shown to be the most effective. 31
ARE THERE INTEGRATIVE HEALTH APPROACHES TO HELP MANAGE CKD?
Studies of the use of complementary and integrative medicine practices have found that anywhere from 23.2%32 to 54.9%33 of patients with CKD use integrative medicine approaches, with the percent increasing in the last few years. As integrative medicine is designed to address the whole person and CKD onset and progression is heavily influenced by lifestyle factors, there are integrative medicine approaches that can help address symptoms and possibly slow CKD disease progression. Additionally, once a patient has reached ESKD and is undergoing hemodialysis, integrative approaches can help address symptoms such as pain, stress, and anxiety.
Please note, before engaging in any of the approaches below, it is important inform your health-care team and discuss how to best integrate these approaches into your CKD-management plan.
ACUPUNCTURE
Acupuncture is a practice in which a trained specialist called an acupuncturist stimulates specific points on the skin called acupoints, usually with a thin needle. Stimulating acupoints increases the release of chemicals like endorphins (naturally produced pain reducers) in the body and brain. These chemicals may directly impact how a person experiences pain.
Side Effects/Safety Concerns
- Slight bleeding and bruising at the acupoint site
- Fainting
- Convulsions (rare)
- Pain or soreness at the acupoint site (which may enhance its effectiveness)
Professionally delivered acupuncture produces only mild and transient side effects in most people. Be sure to find a properly trained and licensed acupuncturist. See the Acupuncture Pocket Guide to help you identify a qualified provider.
Evidence
A systematic review and meta-analysis of 17 randomized controlled trials (including 1,414 participants) on the impact of acupuncture on non-dialysis CKD patients found that acupuncture can reduce blood urea nitrogen and creatine levels, as well as increase creatine clearance and hemoglobin levels. However, the authors caution that the evidence is not sufficient to make treatment recommendations because of the high risk of bias in the included trials. Higher quality research that controls for bias is needed. 34
A prospective observational study of the use of acupuncture for symptom management of CKD patients undergoing hemodialysis reported that after seven weeks of the intervention, acupuncture significantly reduced the patients’ primary symptoms as assessed by the Measure Your Medical Outcome Profiles 2 questionnaire. Acupuncture also produced significant improvement on some subscales of the Kidney Disease Quality of Life–Short Form, such as the burden of kidney disease, physical limitations, emotional well-being, and energy/fatigue. 35
YOGA
Numerous studies attest to the benefits of yoga, a centuries old mind-body practice, on a wide range of health-related conditions—particularly stress, mental health (including depression), and pain management.
Side Effects/Safety Concerns
Although very rare, certain types of strokes, as well as pain from nerve damage, have been reported from people practicing extreme yoga. Muscle injury can also occur if yoga is not practiced properly. Practice yoga under the guidance of a qualified teacher. Minor side effects include:
- Dizziness
- Fatigue
- Weakness
- Nausea
- Heat exhaustion
Evidence
In a controlled study of 54 participants with CKD undergoing regular hemodialysis, 28 participants received usual care and 26 participants received usual care plus a yoga intervention (specifically focused on poses that benefit the kidneys) for six months. The participants were instructed to practice the prescribed yoga intervention at least five times a week for 40 to 60 minutes. Participants in the usual care plus yoga group had a statistically significant decrease in blood pressure and significant improvements in physical and psychological quality of life compared with the group who did not do yoga. 36
A systematic review of two randomized controlled trials (including 68 patients) that looked at the effects of yoga on physical and psychological outcomes in CKD patients on chronic hemodialysis found that the yoga interventions significantly improved quality of life, pain, fatigue, sleep disturbances, and physical function. 37
MOVING MEDITATIONS
Moving meditations (such as Tai Chi and Qigong) build balance, coordination, strength, and functional capacity. They combine the use of slow and deliberate movements with meditation and breathing practices.
Side Effects/Safety Concerns
These practices are widely considered safe ways of addressing physical and mental symptoms; side effects are rare. Minor side effects include aches, pains, and soreness. If you are pregnant, have chronic back problems, or a hernia, please speak with your physician prior to beginning any moving meditation practice.
Evidence
A randomized controlled trial of 21 participants with CKD and cardiovascular disease looked at the impact of a 12-week, 30 minutes per day, two to three times per week Tai Chi intervention. Participants in the intervention group had improved estimated GFR, left ventricular ejection fraction, and high-density lipoprotein levels, and decreased heart rate and systolic blood pressure, diastolic blood pressure, serum creatinine, total cholesterol, triglyceride, and low-density lipoprotein levels. 38
A study, including 46 participants with ESKD, randomized participants to receive usual care alone or usual care plus a once weekly one-hour Tai Chi sessions for 12 weeks. Participants in the Tai Chi program had statistically significant improvements in quality of life and physical functioning. 39
ENERGY HEALING
Energy healing includes a number of different therapeutic interventions, such as Reiki, in which a therapist helps to harness or manipulate a patient’s subtle energy in order to help restore the body’s balance and improve the body’s ability to heal. These “subtle energy” therapeutic interventions have been described and used for thousands of years by traditional Chinese and Indian medicine systems, and also by religious and faith healers through approaches like the laying on of hands.
Side Effects/Safety Concerns
Energy healing is widely considered safe when delivered by a well-trained, certified energy practitioner, provided it is not used as a substitute for a proven treatment. Minor side effects include:
- Increased thirst
- Restlessness
- Anxiety
- Fever
- Mental “spaciness”
Evidence
A pilot study that looked at 15 patients who received Reiki for 20 minutes twice a week for four weeks during hemodialysis found that participants experienced a significant reduction in pain and anxiety. 41
In a pilot study, six participants who were undergoing regular peritoneal dialysis received 10 sessions of healing touch for 30 to 45 minutes. The participants reported improvements in fatigue (decreased by 46%) and pain (decreased by 68%), and reductions in stress/anxiety (decreased by 49%) and depression (decreased by 84%). 41
VITAMINS AND SUPPLEMENTS
Understanding which supplements to take and which to avoid when you have CKD is crucial for maintaining health and preventing further damage to your kidneys. As your disease progresses, your physician and health-care team may recommend adding vitamins and supplements to your treatment plan. Adding vitamins and/or supplements to your routine can help ensure your body maintains a healthy level of important nutrients that are crucial for proper functioning. This is important since you may have to limit your consumption of certain foods that would normally provide you with the nutrients your body needs.
Many of these supplements can be taken in pill form, though some may be injected directly into your body by your physician. However, some vitamins and supplements can cause kidney damage and increase disease progression, so it is imperative that you always speak with your health-care team about the supplements you take and have your GFR and other important indicators monitored.
Vitamins
It is likely your physician may recommend you take the following vitamins at some point during your treatment: 42
- B Complex
- Vitamin B6, B12, and folic acid work together and can help prevent anemia.
- Thiamine, riboflavin, pantothenic acid, and niacin are additional B vitamins that help produce the energy that is needed for the body to function properly.
- Iron can help treat or prevent anemia.
- Vitamin C can keep your tissues healthy, help with wound healing, and can prevent infections. Your vitamin C levels need to be closely monitored because too much vitamin C can increase the excretion of oxalate (a possible toxin) into the kidneys.
- Vitamin D assists with maintaining healthy bones.
- Calcium also assists with maintaining healthy bones. Like vitamin C, calcium levels in the blood should be closely monitored because too much calcium can be harmful.
Vitamins to Avoid
There are certain vitamins that should be avoided because they can build up in the body, speed up disease progression, and be harmful to your health. These include vitamins A, E, and K. These vitamins should only be taken if directed by and closely monitored by your physician.
Additional Supplements
Although not part of the standard practice guidelines, there are other supplements with some research that supports their use. Again, before adding supplements of any kind to your diet, it is important to speak with your health-care providers.
- Omega-3 fatty acids — There is some evidence to support that omega-3 supplements may delay the progression of CKD, reduce the risk of ESKD, and reduce cardiovascular mortality in hemodialysis patients. 43 44
- Curcumin — There is limited evidence supporting the use of curcumin in patients with CKD, but this anti-inflammatory is speculated to help with CKD symptoms and some doctors recommend it. 45
However, curcumin supplements can contain large amounts of potassium, which may be harmful to CKD patients especially in later stages of the disease.
Supplements to Avoid
The National Kidney Foundation recommends that people with CKD and ESKD do not take herbal remedies or OTC nutritional supplements. It is particularly important to avoid the following:
- Saint-John’s-wort — If you are taking immunosuppressants after a kidney transplant, Saint-John’s-wort can significantly interfere with the way the immunosuppressants are metabolized and may cause your body to reject the new organ.
- Salt substitutes that contain a lot of potassium.
- Nutritional supplements that contain a lot of potassium.
- Star fruit (both supplements containing it and the fruit itself) can be fatal for patients with CKD because it contains a neurotoxin that the kidney may not be able to filtrate out of the blood stream. 46
- Stimulants that may raise your blood pressure, which can further damage your kidney over time.
- Supplements that contain aristolochic acid as this can potentially cause nephrotoxicity (toxicity of the kidneys).
To learn more about supplements to avoid, visit the National Kidney Disease Foundation’s Herbal Supplements and Kidney Disease web page.
IN SUMMARY
Conventional approaches to treating CKD involve monitoring your kidney functioning closely with your physician and a team of health-care providers to help you understand your disease and develop routines that will keep your disease from progressing. This includes maintaining a CKD-appropriate diet, exercising regularly, and engaging in self-care activities that will help reduce stress. It is crucial that you closely follow the advice and instructions given by your team of health-care providers after receiving a diagnosis of CKD because with the proper care and attention, your disease may never progress to ESKD, and you may never need dialysis.
Integrative approaches can help manage the symptoms of CKD, reduce the stress of dialysis, and slow disease progression.
It is important to always keep your health-care team informed of the approaches you are interested in integrating into your treatment of CKD as certain strategies may not be appropriate for you and certain supplements can cause damage to your kidneys.
ENDNOTES
- Kidney Disease Statistics for the United States. (2016, December). National Institutes of Diabetes and Digestive and Kidney Diseases. Retrieved February 18,
2021, https://www.niddk.nih.gov/health-information/health-statistics/kidney-disease. - Chronic Kidney Disease in the United States, 2021. (2021, March 4). Chronic Kidney Disease Initiative, Retrieved April 23, 2021, https://www.cdc.gov/kidneydisease/publications-resources/ckd-national-facts.html.
- Kidney Disease: The Basics. (2021). National Kidney Foundation, Retrieved https://www.kidney.org/news/newsroom/fsindex.
- Diabetic Kidney Disease. (2017, February). National Institutes of Diabetes and Digestive and Kidney Diseases. Retrieved February 18, 2021, https://www.niddk.nih.gov/health-information/diabetes/overview/preventing-problems/diabetic-kidney-disease
- Lifestyle Modifications Improve CKD Patient Outcomes. (2015, March 16). National Kidney Foundation. Retrieved April 12, 2021, https://www.kidney.org/news/lifestyle-modifications-improve-ckd-patient-outcomes.
- Chronic Kidney Disease Tests & Diagnosis. (2016, October 1). National Institutes of Diabetes and Digestive and Kidney Diseases. Retrieved March 1, 2021, https://www.niddk.nih.gov/health-information/kidney-disease/chronic-kidney-disease-ckd/tests-diagnosis
- Breyer MD, Susztak K. The next generation of therapeutics for chronic kidney disease. Nat Rev Drug Discov. 2016;15(8):568-588. doi:10.1038/nrd.2016.67
- End Stage Renal Disease (ESRD). (Unknown). John Hopkins Medicine- Health. Retrieved March 1, 2021, https://www.hopkinsmedicine.org/health/conditions-and-diseases/end-stage-renal-failure.
- Managing Chronic Kidney Disease. (2016, October 1). National Institutes of Diabetes and Digestive and Kidney Diseases. Retrieved March 1, 2021, https://www.niddk.nih.gov/health-information/kidney-disease/chronic-kidney-disease-ckd/managing
- Anemia of Chronic Kidney Disease. (2020, December 17). Michigan Medicine, University of Michigan. Retrieved March 1, 2021, https://www.uofmhealth.org/health-library/abr9104.
- Lin, J., Fung, T. T., Hu, F. B., & Curhan, G. C. (2011). Association of dietary patterns with albuminuria and kidney function decline in older white women: a subgroup analysis from the Nurses’ Health Study. American Journal Of Kidney Diseases : The Official Journal of the National Kidney Foundation, 57(2), 245–254. https://doi-org.liboff.ohsu.edu/10.1053/j.ajkd.2010.09.027
- Palmer, S. C., Maggo, J. K., Campbell, K. L., Craig, J. C., Johnson, D. W., Sutanto, B., Ruospo, M., Tong, A., & Strippoli, G. F. (2017). Dietary interventions for adults with chronic kidney disease. The Cochrane database of systematic reviews, 4(4), CD011998. https://doi-org.liboff.ohsu.edu/10.1002/14651858.CD011998.pub2
- Khatri, M., Moon, Y. P., Scarmeas, N., Gu, Y., Gardener, H., Cheung, K., Wright, C. B., Sacco, R. L., Nickolas, T. L., & Elkind, M. S. (2014). The association between a Mediterranean-style diet and kidney function in the Northern Manhattan Study cohort. Clinical journal of the American Society of Nephrology: CJASN, 9(11), 1868–1875. https://doi.org/10.2215/CJN.01080114
- Asghari, G., Farhadnejad, H., Mirmiran, P., Dizavi, A., Yuzbashian, E., & Azizi, F. (2017). Adherence to the Mediterranean diet is associated with reduced risk of incident chronic kidney diseases among Tehranian adults. Hypertension research: Official Journal of the Japanese Society of Hypertension, 40(1), 96–102. https://doi-org.liboff.ohsu.edu/10.1038/hr.2016.98
- Mekki, K., Bouzidi-bekada, N., Kaddous, A., & Bouchenak, M. (2010). Mediterranean diet improves dyslipidemia and biomarkers in chronic renal failure patients. Food & function, 1(1), 110–115. https://doi-org.liboff.ohsu.edu/10.1039/c0fo00032a
- Tyson, C.C, Lin, P., Corsino, L., Batch, B.C., Allen, J., Sapp, S., Barnhart, H., Nwankwo, C., Burroughs, J., Svetkey, L.P. (2016). Short-term effects of the DASH diet in adults with moderate chronic kidney disease: a pilot feeding study. Clinical Kidney Journal, 9(4), pp. 592–598. https://doi-org.liboff.ohsu.edu/10.1093/ckj/sfw046
- Tyson, C. C., Davenport, C. A., Lin, P. H., Scialla, J. J., Hall, R., Diamantidis, C. J., Lunyera, J., Bhavsar, N., Rebholz, C. M., Pendergast, J., Boulware, L. E., & Svetkey, L. P. (2019). DASH Diet and Blood Pressure Among Black Americans With and Without CKD: The Jackson Heart Study. American Journal of Hypertension, 32(10), 975–982. https://doi-org.liboff.ohsu.edu/10.1093/ajh/hpz090
- Hahn, D., Hodson, E. M., & Fouque, D. (2018). Low protein diets for non-diabetic adults with chronic kidney disease. The Cochrane Database of Systematic Reviews, 10(10), CD001892. https://doi-org.liboff.ohsu.edu/10.1002/14651858.CD001892.pub4
- Li, Q., Wen, F., Wang, Y., Li, S., Lin, S., Qi, C., Chen, Z., Qiu, X., Zhang, Y., Zhang, S., Tao, Y., Feng, Z., Li, Z., Li, R., Ye, Z., Liang, X., Liu, S., Xie, J., & Wang, W. (2021). Diabetic Kidney Disease Benefits from Intensive Low-Protein Diet: Updated Systematic Review and Meta-analysis. Diabetes Therapy: Research, Treatment And Education Of Diabetes And Related Disorders, 12(1), 21–36. https://doi-org.liboff.ohsu.edu/10.1007/s13300-020-00952-5
- Hahn, D., Hodson, E. M., & Fouque, D. (2020). Low protein diets for non-diabetic adults with chronic kidney disease. The Cochrane Database of Systematic Reviews, 10, CD001892. https://doi-org.liboff.ohsu.edu/10.1002/14651858.CD001892.pub5
- Exercise: What You Should Know. (2014, March). National Kidney Foundation. Retrieved April 12, 2021, https://www.kidney.org/atoz/content/exercisewyska.
- Barcellos, F. C., Del Vecchio, F. B., Reges, A., Mielke, G., Santos, I. S., Umpierre, D., Bohlke, M., & Hallal, P. C. (2018). Exercise in patients with hypertension and chronic kidney disease: a randomized controlled trial. Journal of Human Hypertension, 32(6), 397–407. https://doi-org.liboff.ohsu.edu/10.1038/s41371-018-0055-0
- Pei, G., Tang, Y., Tan, L., Tan, J., Ge, L., & Qin, W. (2019). Aerobic exercise in adults with chronic kidney disease (CKD): a meta-analysis. International Urology and Nephrology, 51(10), 1787–1795. https://doi-org.liboff.ohsu.edu/10.1007/s11255-019-02234-x
- Zhang, L., Wang, Y., Xiong, L., Luo, Y., Huang, Z., & Yi, B. (2019). Exercise therapy improves eGFR, and reduces blood pressure and BMI in non-dialysis CKD patients: evidence from a meta-analysis. BMC nephrology, 20(1), 398. https://doi-org.liboff.ohsu.edu/10.1186/s12882-019-1586-5
- Choi, N. G., Sullivan, J. E., DiNitto, D. M., & Kunik, M. E. (2019). Associations between psychological distress and health-related behaviors among adults with chronic kidney disease. Preventive Medicine, 126, 105749. https://doi-org.liboff.ohsu.edu/10.1016/j.ypmed.2019.06.007
- Cukor, D., Coplan, J., Brown, C., Friedman, S., Cromwell Smith, A., Peterson, R. A., & Kimmel, P. L. (2007). Depression and anxiety in urban hemodialysis patients. Clinical Journal of the American Society of Nephrology : CJASN, 2(3), 484–490. https://doi-org.liboff.ohsu.edu/10.2215/CJN.00040107
- Park, J., Lyles, R. H., & Bauer-Wu, S. (2014). Mindfulness meditation lowers muscle sympathetic nerve activity and blood pressure in African-American males with chronic kidney disease. American journal of physiology. Regulatory, integrative and comparative physiology, 307(1), R93–R101. https://doi-org.liboff.ohsu.edu/10.1152/ajpregu.00558.2013
- Haghshenas, M., Assarian, F., Omidi, A., Razaghof, M., Rahimi, H. (2019). Efficacy of Mindfulness-based Stress Reduction in Hemodialysis Patients with Anxiety and Depression: a randomized, double-blind, parallel-group trial. Electronic Physician, 11(1), 7370-7377. http://dx.doi.org/10.19082/7370
- Natale, P., Palmer, S. C., Ruospo, M., Saglimbene, V. M., Rabindranath, K. S., & Strippoli, G. F. (2019). Psychosocial interventions for preventing and treating depression in dialysis patients. The Cochrane Database of Systematic Reviews, 12(12), CD004542. https://doi-org.liboff.ohsu.edu/10.1002/14651858.CD004542.pub3
- Sohn, B. K., Oh, Y. K., Choi, J. S., Song, J., Lim, A., Lee, J. P., An, J. N., Choi, H. J., Hwang, J. Y., Jung, H. Y., Lee, J. Y., & Lim, C. S. (2018). Effectiveness of group cognitive behavioral therapy with mindfulness in end-stage renal disease hemodialysis patients. Kidney Research and Clinical Practice, 37(1), 77–84. https://doi-org.liboff.ohsu.edu/10.23876/j.krcp.2018.37.1.77
- Chu, F., Yeam, C. T., Low, L. L., Tay, W. Y., Foo, W., & Seng, J. (2020). The role of Mind-Body Interventions in Pre-dialysis Chronic Kidney disease and Dialysis patients – A Systematic Review of literature. Complementary Therapies in Medicine, 102652. Advance online publication. https://doi-org.liboff.ohsu.edu/10.1016/j.ctim.2020.102652
- AlAnizy, L., AlMatham, K., Al Basheer, A., & AlFayyad, I. (2020). Complementary and Alternative Medicine Practice Among Saudi Patients with Chronic Kidney Disease: A Cross-Sectional Study. International Journal Of Nephrology and Renovascular Disease, 13, 11–18. https://doi-org.liboff.ohsu.edu/10.2147/IJNRD.S240705
- Arjuna Rao, A. S., Phaneendra, D., Pavani, C., Soundararajan, P., Rani, N. V., Thennarasu, P., & Kannan, G. (2016). Usage of complementary and alternative medicine among patients with chronic kidney disease on maintenance hemodialysis. Journalo of Pharmacy & Bioallied Sciences, 8(1), 52–57. https://doi-org.liboff.ohsu.edu/10.4103/0975-7406.171692
- Yang, T., Zhao, J., Guo, Q., Wang, Y., & Si, G. (2020). Acupoint injection treatment for non-dialysis dependent chronic kidney disease: A meta-analysis of randomized controlled trials. Medicine, 99(51), e23306. https://doi-org.liboff.ohsu.edu/10.1097/MD.0000000000023306
- Kim, K. H., Kim, T. H., Kang, J. W., Sul, J. U., Lee, M. S., Kim, J. I., Shin, M. S., Jung, S. Y., Kim, A. R., Kang, K. W., & Choi, S. M. (2011). Acupuncture for symptom management in hemodialysis patients: a prospective, observational pilot study. Journal Of Alternative and Complementary Medicine (New York, N.Y.), 17(8), 741–748. https://doi-org.liboff.ohsu.edu/10.1089/acm.2010.0206
- Pandey, R. K., Arya, T. V., Kumar, A., & Yadav, A. (2017). Effects of 6 months yoga program on renal functions and quality of life in patients suffering from chronic kidney disease. International Journal of Yoga, 10(1), 3–8. https://doi-org.liboff.ohsu.edu/10.4103/0973-6131.186158
- KauricKlein Z. (2019). Effect of yoga on physical and psychological outcomes in patients on chronic hemodialysis. Complementary Therapies in Clinical Practice, 34, 41–45. https://doi-org.liboff.ohsu.edu/10.1016/j.ctcp.2018.11.004
- Shi, Z. M., Wen, H. P., Liu, F. R., & Yao, C. X. (2014). The effects of tai chi on the renal and cardiac functions of patients with chronic kidney and cardiovascular
diseases. Journal of Physical Therapy Science, 26(11), 1733–1736. https://doi-org.liboff.ohsu.edu/10.1589/jpts.26.1733 - Chang, J. H., Koo, M., Wu, S. W., & Chen, C. Y. (2017). Effects of a 12-week program of Tai Chi exercise on the kidney disease quality of life and physical functioning of patients with end-stage renal disease on hemodialysis. Complementary Therapies in Medicine, 30, 79–83. https://doi-org.liboff.ohsu.edu/10.1016/j.ctim.2016.12.002
- Zins, S., Hooke, M. C., & Gross, C. R. (2019). Reiki for Pain During Hemodialysis: A Feasibility and Instrument Evaluation Study. Journal Of Holistic Nursing: Official Journal of The American Holistic Nurses’ Association, 37(2), 148–162. https://doi-org.liboff.ohsu.edu/10.1177/0898010118797195
- Hendricks, K., & Wallace, K. F. (2017). Pilot Study: Improving Patient Outcomes with Healing Touch. Advances in peritoneal dialysis. Conference on Peritoneal
Dialysis, 33(2017), 65–67. - 42 Vitamins and Minerals in Chronic Kidney Disease. (2019, May 31). National Kidney Foundation. Retrieved, April 12, 2021, https://www.kidney.org/atoz/content/vitamineral.
- Hu, J., Liu, Z., & Zhang, H. (2017). Omega-3 fatty acid supplementation as an adjunctive therapy in the treatment of chronic kidney disease: a meta-analysis. Clinics (Sao Paulo, Brazil), 72(1), 58–64. https://doi.org/10.6061/clinics/2017(01)10
- Saglimbene, V. M., Wong, G., van Zwieten, A., Palmer, S. C., Ruospo, M., Natale, P., Campbell, K., Teixeira-Pinto, A., Craig, J. C., & Strippoli, G. (2020). Effects of omega-3 polyunsaturated fatty acid intake in patients with chronic kidney disease: Systematic review and meta analysis of randomized controlled trials. Clinical Nutrition (Edinburgh, Scotland), 39(2), 358–368. https://doi-org.liboff.ohsu.edu/10.1016/j.clnu.2019.02.041
- Ghosh, S. S., Gehr, T. W., & Ghosh, S. (2014). Curcumin and chronic kidney disease (CKD): major mode of action through stimulating endogenous intestinal alkaline phosphatase. Molecules (Basel, Switzerland), 19(12), 20139–20156. https://doi-org.liboff.ohsu.edu/10.3390/molecules191220139
- Why You Should Avoid Earing Starfruit. (2021). National Kidney Foundation. Retrieved June 17, 2021, https://www.kidney.org/atoz/content/why-you-should-avoid-eating-starfruit
Topics: Chronic Disease | Integrative Health
