Co-authored by Genevieve Walker, PhD, a medical writer with more than 15 years of medical writing experience and 25 years of healthcare experience.
Your guide to coping with hot flashes, weight gain, period changes and more
Should your 40s come with a warning label?
Angela thinks so. “As soon as I turned 40, I couldn’t eat the same way I used to,” she says. “I gained weight if I so much as looked at a French fry.” Always slender, she had to exercise more to fit into the same clothes and – suddenly – watch what she ate.
Weight gain, hot flashes, and night sweats … oh my!
Jamie agrees about the warning label but for different reasons. She had her first hot flash while taking a business call in her home office. It was a warm day, so she was already a bit overheated. Suddenly, her dog began barking in another room. Quickly, Jamie stepped onto the balcony and closed the door. It was quieter but much warmer outdoors. Jamie felt her face, neck, and chest flushing, and she began dripping sweat.
“Thank goodness it wasn’t a video call,” she remembers. “The warm day, sudden stress, and stepping into an even warmer environment created the perfect storm. I realized that at age 45, I had just experienced my very first hot flash.”
She soon learned she was not alone. Her friend Shannon, 46, described waking up in soggy sheets with damp hair sticking to her neck. “Night sweats” is the common term for nocturnal hot flashes.
With the average age of menopause at 51, the 40s are usually when perimenopause starts. But this phase can take between four and 10 years. Most women notice changes in their periods, like Cynthia did before her menstrual cycles stopped at age 53.
“At first, the time between periods shortened. I had a period about every three weeks,” she recalls. “Then, it stretched out. I could go one, two, even three or four months without a period, or just have a little light bleeding [spotting]. Once, I went almost a full year with no bleeding [the sign doctors use to determine when a woman has reached menopause]. Then I had a period again.”
Hot flashes: the integrative approach
From the 1960s through the early 2000s, many women started taking pills that combined estrogen and progesterone around the time of perimenopause – and kept taking them almost indefinitely. However, research from a major study called the Women’s Health Initiative changed that in 2002, when the standard hormone replacement therapy regimen was found to raise the risk of heart disease, breast cancer, and other serious health problems.[i]
In time, doctors were able to separate the risks of this treatment from the benefits and determine which women could still safely take hormones for their symptoms. Now called menopause hormone therapy (MHT), this treatment is still an option for many women. However, many women are looking for non-hormonal options.
At the most basic level, a non-drug approach to hot flashes starts with keeping your cool, literally. Carrying a portable fan, setting your thermostat lower, dressing in light layers, and, for night sweats, choosing wicking material for pajamas and bedding can help you maintain a more comfortable body temperature and avoid triggering a hot flash. There are even cooling gel mattresses and pillow inserts to help you sleep better.[ii]
Integrative health options for hot flashes
The North American Menopause Society (NAMS) is a reliable, patient-friendly resource for information on every phase of this transition, including perimenopause supplements. The NAMS guide to natural remedies for hot flashes covers black cohosh, red clover, dong quai (angelica), ginseng, kava, and evening primrose oil.[iii] Takeaways include:
- Black cohosh and red clover may help some women, but the evidence is not yet conclusive, and they may also contribute to liver problems and cancer.
- Kava, evening primrose oil, and dong quai can all cause serious side effects, and the evidence is not conclusive that they help hot flashes.
- Ginseng can be helpful for other perimenopause issues, such as mood and sleep, but does not appear to be especially helpful for hot flashes.
A review of natural menopause treatments by Baylor University researchers found that hypnosis and aromatherapy with lavender oil can effectively relieve hot flashes.[iv] They also found that black cohosh supplements and reflexology, a massage technique that stimulates specific points on the feet and hands, can help.
Cognitive-behavioral-therapy, a type of short-term, focused counseling, does not appear to reduce the frequency of hot flashes, but it may make them less bothersome.
More research needed for other perimenopause supplements and treatments
What’s the worry about non-FDA-approved treatments?
Concerns about unproven natural remedies include:
- Side effects, sometimes serious.
- Being undertreated, meaning the treatment is not strong enough to effectively manage your symptoms when a proven treatment would be.
Mindfulness-based stress reduction, techniques that help you relax and focus on the moment, appear to be more helpful with other perimenopause symptoms, such as reducing anxious feelings and increasing your sense of well-being, than with hot flashes. This treatment may also help increase energy levels, as can yoga. For other treatments, more research is needed to learn if they are genuinely effective and safe to manage hot flashes. These “need more information” treatments include relaxation therapy, maca supplements, flower pollen extract, homeopathy, acupuncture, and traditional Chinese medicine treatments.[iv]
To learn more about integrative approaches to hot flashes and other symptoms common in menopause and perimenopause, download our free guide.
Bioidentical and over-the-counter perimenopause supplements
Several celebrities have endorsed using “bioidentical” hormone therapy: treatments created specifically for you at a pharmacy or developed for general sale. Your health care provider can help you make sure what you choose to do is safe, worth the cost, and unlikely to interact with other medications or supplements you take.
They can also prescribe a bioidentical hormone preparation, such as an estrogen cream for vaginal dryness and urinary symptoms.
Managing perimenopause weight gain
“How to lose weight” is one of the most searched topics related to perimenopause. But why do we tend to gain weight at this age? A study published in the Journal of Mid-Life Health lists contributing factors,[v] including:
- Loss of muscle mass as we get older, coupled with a slower metabolism and more sedentary lifestyle.
- Stress and emotional eating.
- A diet high in fat, sugar, salt, and processed foods, and low in fiber.
- Poor sleep.
- Drinking too much alcohol.
The researchers recommend:
- Eating plenty of calcium, iron, magnesium, and vitamins. Explore whether you may need supplements or testing for vitamin deficiencies.
- Avoiding spicy foods, alcohol, and caffeine to reduce hot flashes.
- Getting 150 minutes of moderate physical activity per week, such as walking, running, swimming, or cycling, plus strength training two or three times a week to help maintain muscle mass. Being stick thin is not the goal; being your healthiest, including preventing or delaying bone loss and keeping your heart healthy, definitely is.
- Practicing yoga, stretching, and balance exercises to help maintain flexibility and general health.
Maintaining a weight that you and your doctor or nurse agree is appropriate for your height can help you avoid hot flashes after your periods stop (post-menopause hot flashes). In perimenopause, managing your weight can also help you avoid other symptoms.[vi]
Our free Integrative Health Self-Care Guide gives you a program for maintaining basic good health that will have you feeling happier, healthier, more confident and fit even if your weight rises slightly during the transition to menopause.
Keep the conversation going
Of course, always talk with your doctor or other health care provider before trying any new treatment, exercise program, supplement, or nutritional approach. Something that works well for a friend or even a close relative may not work for you, may cause annoying or dangerous side effects, or may interact with medication or supplements that you are already taking.
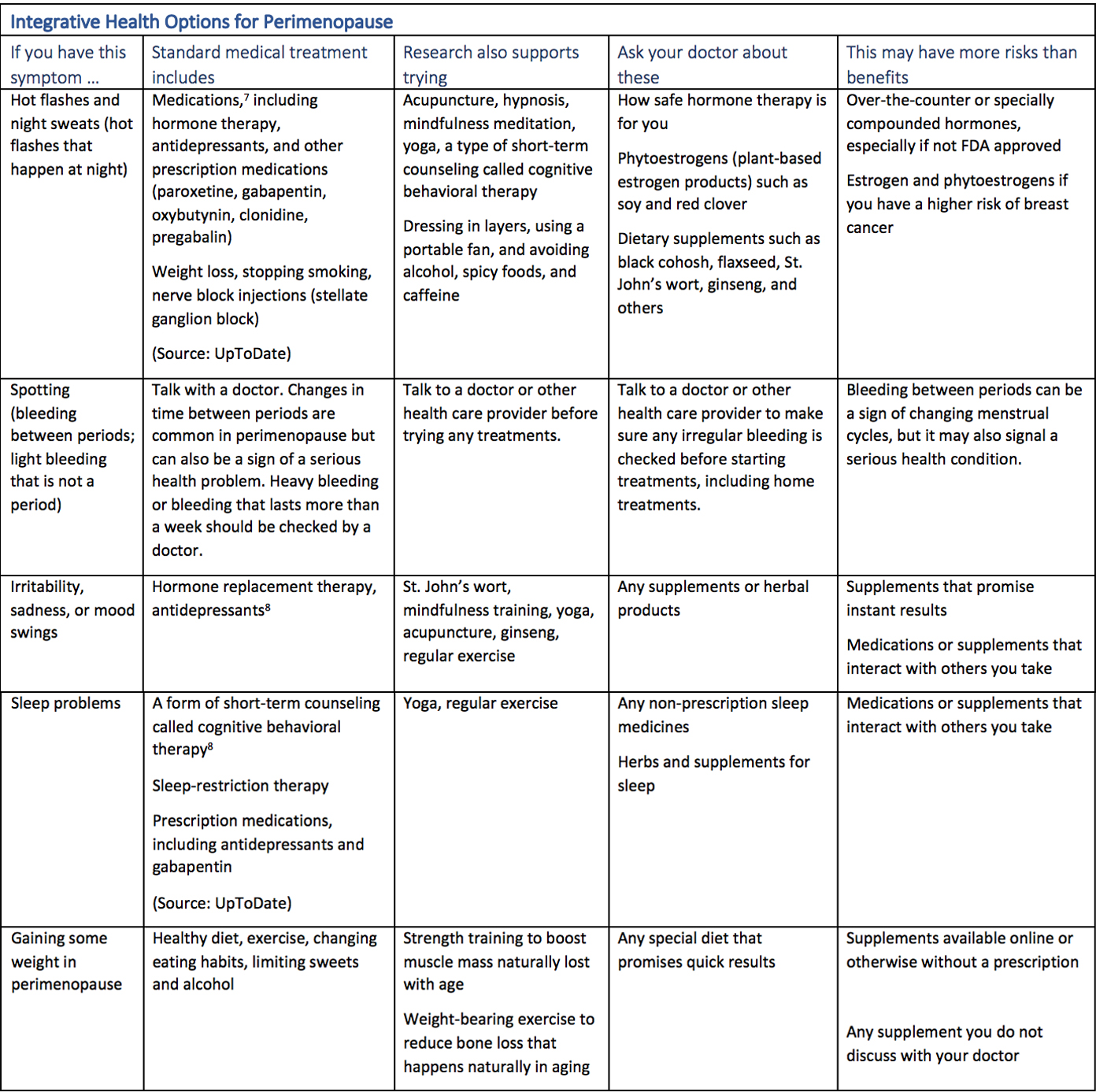
Your quick guide to integrative perimenopause options
Final word: the placebo effect
Many reviews of integrative treatments for perimenopause symptoms compare the treatment to a simulated treatment that may look or feel the same but does not contain the substance being studied. In many cases, the integrative treatment and placebo are about equally effective. But this does not mean we should discount the power of the “placebo effect,” where a simulated treatment actually helps the condition. Learn how receiving a treatment that has meaning for you can produce real improvements.
This article is part of a series dedicated to perimenopause. Read our previous article, “Peri-what? Know Your Perimenopause.”
References
[i] Rossouw JE, Anderson GL, Prentice RL, LaCroix AZ, Kooperberg C, Stefanick ML, Jackson RD, Beresford SA, Howard BV, Johnson KC, Kotchen JM, Ockene J; Writing Group for the Women’s Health Initiative Investigators. Risks and benefits of estrogen plus progestin in healthy postmenopausal women: principal results From the Women’s Health Initiative randomized controlled trial. JAMA. 2002 Jul 17;288(3):321-33. doi: 10.1001/jama.288.3.321. PMID: 12117397
[ii] How to find relief from hot flashes at night. Cleveland Clinic Health Essentials. Available at https://health.clevelandclinic.org/how-to-find-relief-for-hot-flashes-at-night/. Accessed June 1, 2021
[iii] Natural remedies for hot flashes. North American Menopause Society. Available at https://www.menopause.org/for-women/menopauseflashes/menopause-symptoms-and-treatments/natural-remedies-for-hot-flashes. Accessed June 1, 2021
[iv] Johnson A, Roberts L, Elkins G. Complementary and Alternative Medicine for Menopause. Journal of Evidence-Based Integrative Medicine. January 2019. doi:1177/2515690X19829380
[v] Chopra S, Sharma KA, Ranjan P, Malhotra A, Vikram NK, Kumari A. Weight management module for perimenopausal women: A practical guide for gynecologists. J Midlife Health. 2019 Oct-Dec;10(4):165-172. doi: 10.4103/jmh.JMH_155_19. PMID: 31942151; PMCID: PMC6947726
[vi] Koo, S., Ahn, Y., Lim, JY. et al. Obesity associates with vasomotor symptoms in postmenopause but with physical symptoms in perimenopause: a cross-sectional study. BMC Women’s Health 17, 126 (2017). https://doi.org/10.1186/s12905-017-0487-7
[vii] Santen RJ, Loprinzi CL, Casper RF. Menopausal hot flashes. Available at https://www.uptodate.com/contents/menopausal-hot-flashes?search=perimenopause%20muscle%20mass&topicRef=7395&source=see_link#H51257202. Updated April 27, 2020; literature review current through May 2021
[viii] Casper RF. Clinical manifestations and diagnosis of menopause. UpToDate. Available at https://www.uptodate.com/contents/clinical-manifestations-and-diagnosis-of-menopause?source=history_widget#H172092817. Updated March 20, 2021; literature review current through May 2021
Take Your Health Into Your Own Hands
Drawing on 40 years of research and patient care, Dr. Wayne Jonas explains how 80 percent of healing occurs organically and how to activate the healing process.